‘New lease on life’ | by

Aurora doctors offer minimally-invasive heart-valve replacement to otherwise option-less patients
Heart-valve replacement surgery, one of the most common surgeries cardiac surgeons perform, can restore quality of life and add years to survival. But it requires open-heart surgery, an option some patients refuse out of fear and other patients are denied due to prohibitive risk. This fall, doctors at The Medical Center of Aurora began offering the first minimally-invasive aortic valve-replacement procedure for qualifying HealthONE patients, giving some people the life-extending option through only a small puncture in their groin.
Called TAVR (transcatheter aortic valve implantation), the procedure involves threading a compressed cow valve through a catheter, inserted through the groin, and opening it inside the old valve, where it takes over the failing valve’s job. Dr. Jonathan Sherman, an interventional cardiologist, and Dr. Jason Sperling, a cardiac surgeon ̶ along with their TMCA Heart Team ̶ began offering TAVR together in October for high-risk or inoperable aortic-stenosis patients.
What is aortic stenosis?
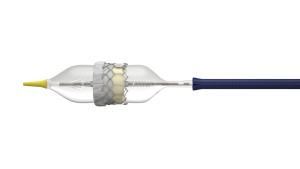
The Edwards SAPIEN 3 transcatheter heart valve expands into place in the heart with the help of an inflatable balloon catheter.
Dr. Sperling: It’s basically a degeneration of the main heart valve, which separates the main squeezing chamber of the heart, the left ventricle, from the rest of the body. Its job is to open up wide to let the blood get ejected out of the heart and also to close tightly so that blood doesn’t leak backward into the heart. This valve is a work-horse that is getting beat up throughout a person’s lifetime. Many people’s aortic valves are going to get a little bit thicker over time, which can lead to restriction or calcification. That’s age-related aortic stenosis.
Can it be detected early and progression slowed?
Dr. Sperling: It can be detected fairly early by listening for a murmur, an abnormal heart sound that is created by turbulent blood flow across the valve. Progression is expected and probably unavoidable. There is no medication that can treat it. It’s not like you can exercise or eat better to prevent it. Eventually, it will probably require treatment.
Once it reaches the severe state, what is the survival rate?

The Edwards SAPIEN 3 transcatheter heart valve is constructed of bovine pericardial leaflets, from the durable sac of tissue surrounding a cow’s heart, hand sewn onto a metal frame that is crimped onto a balloon-expandable catheter. The heart valve has an outer sealing skirt is designed to prevent paravalvular leak.
Dr. Sperling: It’s said that patients who have severe symptomatic aortic stenosis have a two-year survival rate of about 50 percent without surgery, which is really dramatic. Very few conditions have only a 50-percent two-year survival, not even some advanced cancers.
And with surgery?
Dr. Sperling: That can depend on a lot of things. It depends on how old you are; it depends on what other medical problems you have. But, it’s typically much, much better than just observation.
How often do you see patients with this problem?
Dr. Sherman: It’s one of the more-common diagnoses that we see. And, as our population is getting older, and people are living longer, we are seeing more cases and more severe case. In my practice, we’re seeing at least several patients a week.
When you see people in this severe state, what are their lives like?
Dr. Sperling: They can become easily winded and unable to do every-day activities. Sometimes dizziness, fainting, leg swelling and chest pain can occur, generally in later stages. Low energy can have a huge effect on quality of life, and there is a risk of sudden death.
Why might TAVR be a better option for some patients?
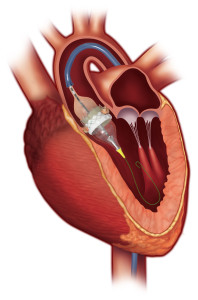
The Edwards SAPIEN 3 transcatheter heart valve expands into place in the heart with the help of an inflatable balloon catheter.
Dr. Sherman: For some high-risk patients, TAVR is the only option. It’s about offering a good therapy to patients who might not have had any therapy offered to them at all. Right now, Medicare has restricted TAVR to high-risk patients or patients who are “inoperable,” who cannot have the traditional valve surgery for some reason. Our hope is that, with newer data coming out on TAVR-patient outcomes even this year, Medicare might begin covering the procedure for intermediate-risk patients. With TAVR, we don’t have to open the chest, patients don’t have to go on a heart-and-lung machine, and hospital stays and recovery times can be much shorter.
Do TAVR patients have the option of either a mechanical or a biological valve?
Dr. Sperling: TAVRs are only biological; they are all tissue valves, which is actually better for patients, because they don’t have to be on major blood thinners or other medications to reduce the risk of clotting.
Why is your team approach important?
Dr. Sperling: It’s all about the complementary skill-sets: We each bring different expertise to the table. I think the patients benefit dramatically from this multidisciplinary team approach, and I think it’s the future in cardiovascular care.
How has TAVR helped your patients?
Dr. Sherman: For some patients, we can help them live longer and do the things they want to do again. A patient we saw yesterday, he is 30 days out from having his TAVR done, and he was just ecstatic. He would not have been doing so well 30 days after open-heart surgery, and we are so happy we had this less-invasive therapy to offer him. He’s back to exercising, doing things with his family, and looking forward to traveling. As he put it, he has a whole new lease on life.
Appointments: 303-597-4239 | Visit: AuroraMed.com/TAVR
Tags: TAVR (transcatheter aortic valve implantation)
Leave a Comment
Please be respectful while leaving comments. All comments are subject to removal by the moderator.


