Not Your Mother’s Cholesterol Screening | by
Everything you need to know about cholesterol, now
In spite of what you may think or have heard, cholesterol is not a bad thing. In fact, cholesterol is a necessary blood chemical that our body produces to make hormones, vitamin D, and help with digestion. Another thing you may have heard is that a total high cholesterol number is bad. Period.
New American College of Cardiology (ACC) guidelines on cholesterol management issued in 2018 recommends looking beyond the number. “Before these new guidelines, it was very black and white. If your number was too high, you went on medication,” explains Dr. TianChu Shih, a double board-certified cardiologist and internist at Lone Tree Internal Medicine at Sky Ridge Medical Center in Lone Tree.
Now cardiologists and internists are looking at, what Shih calls, the good, the bad and the ugly, and also your health and lifestyle risk factors when it comes to how cholesterol fits into a long-term risk management picture for cardiovascular and overall health.
What we want to do is focus on primary prevention for someone who doesn’t have coronary artery disease, cardiovascular disease, or stroke… We focus on what we can do to prevent these diseases.”
The Good, The Bad and The Ugly
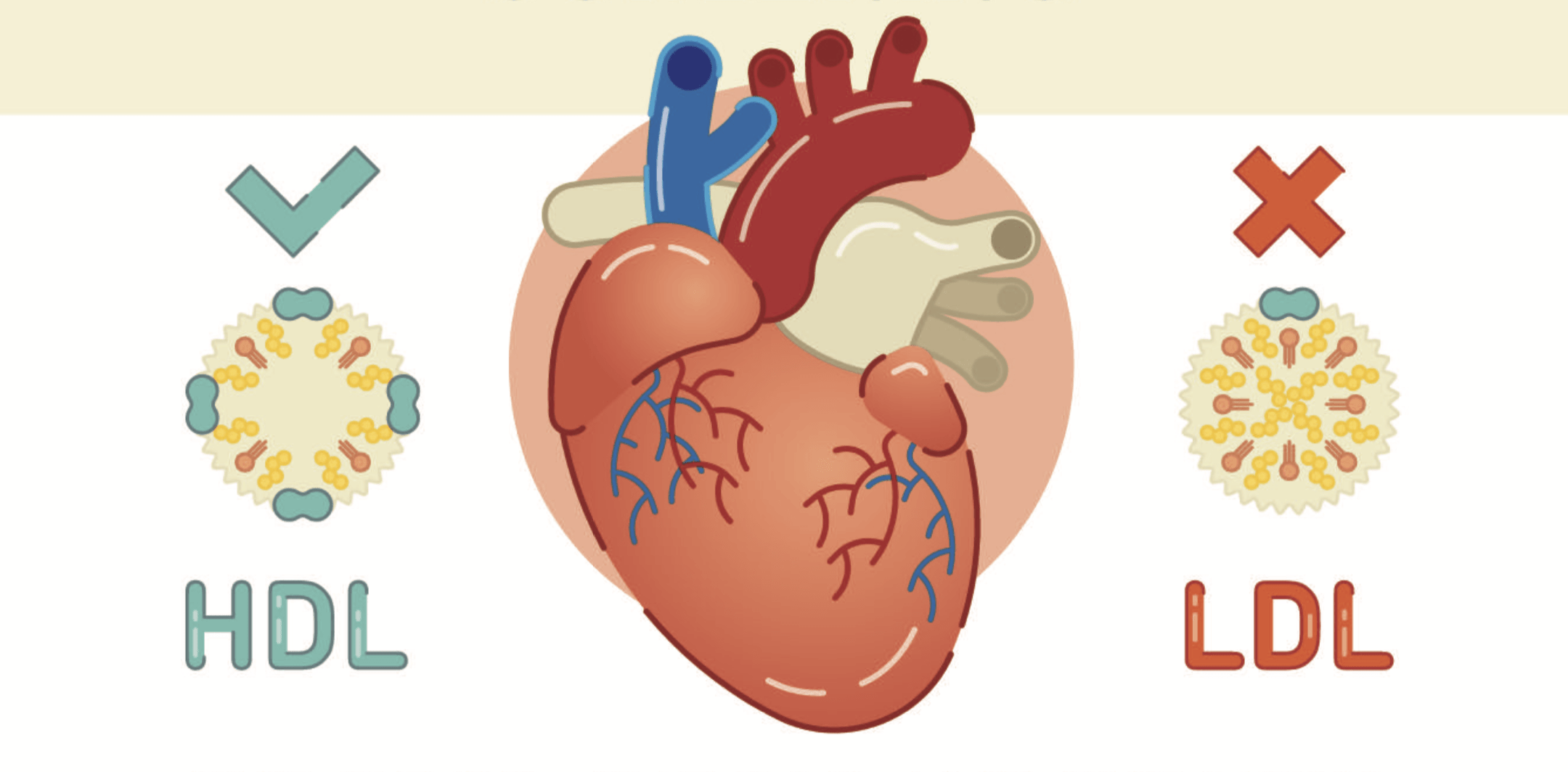
By “the good,” Shih is referring to high-density lipoprotein, or HDL, because it acts as a scavenger by eliminating the bad cholesterol from your system. Bad cholesterol, called low-density lipoprotein, or LDL, is the cholesterol that can turn into plaque buildup and, eventually, restrict blood flow to important organs, most notably your heart.
The ugly part of your lipid panel is high triglycerides. While not as important as your HDL and LDL in terms of heart attack and stroke prevention, triglyceride levels should not be ignored. Nearly a third of all adults have elevated levels of this ugly cholesterol. “High triglycerides increase your risk for diabetes and acute pancreatitis,” explains Shih. High triglycerides can also indicate metabolic syndrome, which does increase your risk for coronary artery disease.
More Than a Number

“We need to ask more questions of the patient to really get an idea of what their risk assessment is,” says Palmquist. “If you handed me a lipid panel and didn’t tell me anything else, I would have no idea what we would need to do for that particular person, how aggressive we would need to be with regards to diet and medications.”
Palmquist says that in addition to your diet, your family history, health history, blood pressure, smoking history, and weight are all part of your overall risk assessment. For example, having diabetes or an inflammatory disease such as lupus or rheumatoid arthritis can raise your risk. Having had a previous heart attack or stroke increases your risk. Two people with a similar lipid panel where one has diabetes would most likely receive different risk assessments and treatment recommendations.
Doctors now take all this information and present their patients with an ASCVD, or atherosclerotic cardiovascular disease, 10-year risk assessment which helps you and your doctor minimize your risks for stroke and heart attack, the two biggest causes of death in the United States.
Cholesterol: Not Just Bad for Your Heart
If your body does have too much cholesterol, which is a waxy substance that floats in your bloodstream, it joins with other substances to form plaque. Plaque is a sticky substance that attaches to the walls of your arteries. Plaque buildup is called atherosclerosis, which is most commonly associated with cardiovascular issues.
However, high cholesterol and plaque can affect any artery in your body. “You could get plaque in the arteries that go to the kidneys and get renal artery disease,” says Palmquist. “You can get plaque in your legs and develop peripheral arterial disease, which could lead to ulcers, sores, and even amputation.”
Blocked blood flow due to high cholesterol, or other reasons, can lead to erectile dysfunction as well. And then there’s the saying, what’s good for your heart is good for your brain. Keeping your cholesterol down can help keep the tiny arteries to your brain healthy. Several studies tie high cholesterol to dementia, so keeping it low and your arteries clear can only help the blood flow to your brain as well as your cognitive function.
Prevention is Key
After age 40, your 10-year ASCVD risk assessment will dictate how often you have your levels and risk factors checked. For those with a family history of cardiovascular disease, other chronic health conditions, or elevated, your schedule may vary.
“What we want to do is focus on primary prevention for someone who doesn’t have coronary artery disease, cardiovascular disease, or stroke. Those are the vast majority of my patients,” says Shih. “We focus on what we can do to prevent these diseases.”
Two main areas of focus are diet and exercise. Both Shih and Palmquist recommend cutting back on red meat and saturated fats and increasing your intake of vegetables, fruits, whole grains, low-fat dairy, and salmon.
Shih likes the anti-inflammatory diet, which she describes as a modified Mediterranean diet. “It’s targeting heart attack and stroke but also cancer, arthritis, depression, and dementia.” Palmquist suggests a Mediterranean-style diet or the DASH (dietary approach to stop hypertension) diet for heart health, or South Beach Diet for those who need more rigid guidelines.
As for exercise, try to move and get your heart rate up for at least 30 minutes on most days. You don’t need a fancy workout or gym time. Walking or dancing will do the trick. Shih warns that weight lifting does not count toward cardiovascular exercise, plus, too much of it can increase the muscles around your heart. But high reps of light weights are ok, she says.
If diet and exercise don’t help improve your risk profile after three months, your doctor may recommend medication.
Tags: Heart Health, Sky Ridge
Comments
Leave a Comment
Please be respectful while leaving comments. All comments are subject to removal by the moderator.

I am looking for Dr. Shih. She is currently listed in Lonetree Internal Medicine and they do not know where she is at. She is the best Dr. I have ever had and I am trying to find her. Can you help?
Hi Lynn, It appears Dr. Shih has left Lone Tree Internal Med. I called the front office and reception does not know where she moved her practice. Sorry I can’t help. Pete